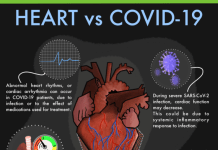
Recente tweelingstudies hebben nieuwe manieren aangetoond om een beschadigd hart te regenereren
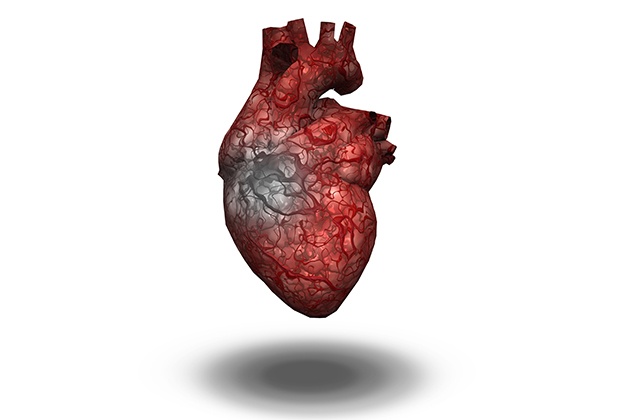
Hartfalen treft wereldwijd minstens 26 miljoen mensen en is verantwoordelijk voor talloze dodelijke sterfgevallen. Door de toenemende vergrijzing is het zorgen voor de hart- Het wordt een noodzaak die leidt tot stijging van de uitgaven. Er is aanzienlijke vooruitgang geboekt op het gebied van therapeutische behandelingen voor de hart- en er worden veel preventieve maatregelen genomen, maar de mortaliteit en morbiditeit zijn nog steeds erg hoog. Er zijn zeer weinig behandelingsopties beschikbaar en meestal berust het op harttransplantatie voor de patiënten die zich echt in het eindstadium bevinden en op weg zijn naar volledig hartfalen.
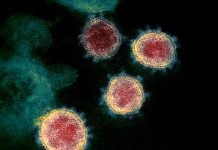
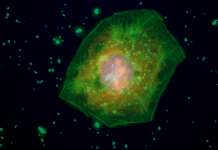
Ons lichaam heeft een buitengewoon vermogen om zichzelf te genezen; de lever kan bijvoorbeeld worden geregenereerd als deze beschadigd is, onze huid meestal ook en één nier kan de functie van twee nieren overnemen. Helaas geldt dit niet voor de meeste van onze vitale organen, inclusief het hart. Wanneer een menselijk hart beschadigd raakt – veroorzaakt door een ziekte of letsel – is de schade eeuwigdurend. Na een hartaanval kunnen bijvoorbeeld miljoenen of miljarden hartspiercellen voor altijd verloren gaan. Dit verlies verzwakt het hart geleidelijk en leidt tot ernstige aandoeningen zoals hartfalen of littekens in het hart die fataal kunnen zijn. Hartfalen ontstaat meestal als er een tekort aan hartspiercellen (type cellen) ontstaat. In tegenstelling tot salamanders en salamanders kunnen volwassen mensen niet spontaan beschadigde organen zoals het hart terug laten groeien. In een menselijk embryo of wanneer een baby in de baarmoeder groeit, hart- cellen delen en vermenigvuldigen zich, waardoor het hart negen maanden lang kan groeien en ontwikkelen. Maar zoogdieren, inclusief mensen, bezitten niet het vermogen om het hart te regenereren, aangezien ze dit vermogen vervolgens en volledig verliezen na ongeveer een week na de geboorte. Hartspiercellen verliezen hun vermogen om te delen en te vermenigvuldigen en kunnen daarom niet regenereren. Dit geldt ook voor andere menselijke cellen – hersenen, spinal cord enz. Aangezien deze volwassen cellen zich niet kunnen delen, kan het menselijk lichaam de beschadigde of verloren gegane cellen niet vervangen en dit leidt tot ziekten. Hoewel dit ook de reden is waarom er nooit een harttumor is, worden tumoren veroorzaakt door ongecontroleerde groei van cellen. Als het echter mogelijk wordt gemaakt dat deze cellen zich weer gaan delen, kan dit leiden tot 'regeneratie' van een aantal weefsels en helpen bij het herstel van een orgaan.
De enige optie die iemand heeft als hij lijdt aan een zwakke of beschadigd hart of een hartaandoening is om een harttransplantatie te ondergaan. Dit heeft een groot aantal aspecten die er doorgaans voor zorgen dat een transplantatie bij de meeste patiënten geen realiteit wordt. Ten eerste moet het hart dat door een “donor” wordt gedoneerd een gezond hart zijn voordat de donor overleed, wat betekent dat het hart moet worden geoogst van jonge mensen die zijn overleden als gevolg van ziekte of verwondingen en deze omstandigheden geen invloed hebben gehad op hun leven. hart- In elk geval. De potentiële ontvangende patiënt moet matchen met het donorhart om de transplantatie te ontvangen. Dit vertaalt zich in een lange wachttijd. Als mogelijk alternatief zou het potentieel om via celdeling nieuwe spieren in het hart te kunnen creëren, hoop kunnen bieden aan miljoenen mensen met een beschadigd hart. Veel procedures zijn door de wetenschappelijke gemeenschap beproefd en getest, maar de resultaten tot nu toe zijn niet effectief geweest.
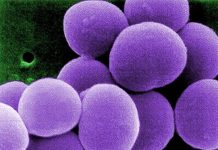
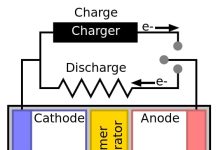
In een nieuwe studie gepubliceerd in Cel, onderzoekers van de Universiteit van Californië, San Francisco, VS hebben voor het eerst een efficiënte en stabiele methode in diermodellen ontwikkeld om volwassen hartcellen (cardiomyocyten) te laten delen en zo mogelijk het beschadigde deel van het hart te herstellen1. De auteurs identificeerden vier genen die betrokken zijn bij celdeling (dat wil zeggen cellen die zich zelfstandig vermenigvuldigen). Toen deze genen werden gecombineerd met genen die ervoor zorgen dat volwassen hartspiercellen opnieuw een celcyclus binnengaan, zagen ze dat cellen zich gingen delen en reproduceren. Dus toen de functie van deze vier essentiële genen werd verbeterd, werd de hart- weefsel vertoonde regeneratie. Na hartfalen bij een patiënt verbetert deze combinatie de hartfunctie. Cardiomyocyten vertoonden een deling van 15-20 procent in het huidige onderzoek (vergeleken met 1 procent in eerdere onderzoeken), wat de betrouwbaarheid en efficiëntie van dit onderzoek bevestigde. Deze studie zou technisch gezien kunnen worden uitgebreid naar andere organen, omdat deze vier genen een gemeenschappelijk kenmerk zijn. Dit is een zeer relevant werk, omdat elke studie over de hart- is ten eerste erg ingewikkeld en ten tweede moet de afgifte van genen met voorzichtigheid gebeuren om geen tumoren in het lichaam te veroorzaken. Dit werk zou kunnen uitmonden in een zeer krachtige aanpak voor het regenereren van het hart en ook andere organen.
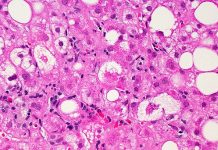
Een ander onderzoek door het Stem Cell Institute van de Universiteit van Cambridge, VK, heeft een innovatieve manier van repareren ontwikkeld hart- zodanig weefsel dat er helemaal geen donor nodig zou zijn2. Ze hebben stamcellen gebruikt om in het laboratorium levende stukjes ‘hartspier’ te laten groeien, die slechts 2.5 vierkante centimeter groot zijn, maar ze lijken een krachtig potentieel hulpmiddel om patiënten met hartfalen te behandelen. Deze pleisters hebben een goed vooruitzicht om op natuurlijke wijze te worden opgenomen in die van een patiënt hart- dat wil zeggen dat het een “volledig functioneel” weefsel is dat net als een normale hartspier klopt en samentrekt. Een eerdere aanpak waarbij stamcellen in het lichaam werden geïnjecteerd om het hart te herstellen, was niet succesvol omdat de stamcellen niet in het lichaam bleven hart- spier, maar ging in plaats daarvan verloren in het bloed. De huidige pleister is een ‘levend’ en ‘kloppend’ hartweefsel dat aan een orgaan kan worden bevestigd (in dit geval de hart-) en zo kon eventuele schade worden gerepareerd. Dergelijke pleisters kunnen worden gekweekt als er vraag is naar een patiënt. Dit zou in wezen de noodzaak om te wachten op een passende donor te boven gaan. Deze plekken kunnen ook worden gekweekt met behulp van de hart- de eigen cellen van de patiënt, waardoor de risico's die gepaard gaan met orgaantransplantatie worden geëlimineerd. Het assimileren van de patch in een beschadigd hart is een invasieve procedure en vereist correcte elektrische impulsen voor het maken van de hart- beat goed geïntegreerd met een patch. Maar de risico's die aan dit soort procedures verbonden zijn, zijn groter dan die van een totale harttransplantatie, die veel invasiever is. Het team bereidt zich voor op dierproeven en klinische proeven binnen vijf jaar voordat dit op grote schaal kan worden gebruikt hart- patiënten.
***
{U kunt de originele onderzoekspaper lezen door op de DOI-link hieronder in de lijst met geciteerde bron(nen) te klikken}
Bron (nen)
1. Mohamed et al. 2018,. Regulering van de celcyclus om de proliferatie van volwassen cardiomyocyten en hartregeneratie te stimuleren. Cel. https://doi.org/10.1016/j.cell.2018.02.014
2. Universiteit van Cambridge 2018. Een gebroken hart oplappen. http://www.cam.ac.uk/research/features/patching-up-a-broken-heart. [Toegang tot 1 mei 2018]